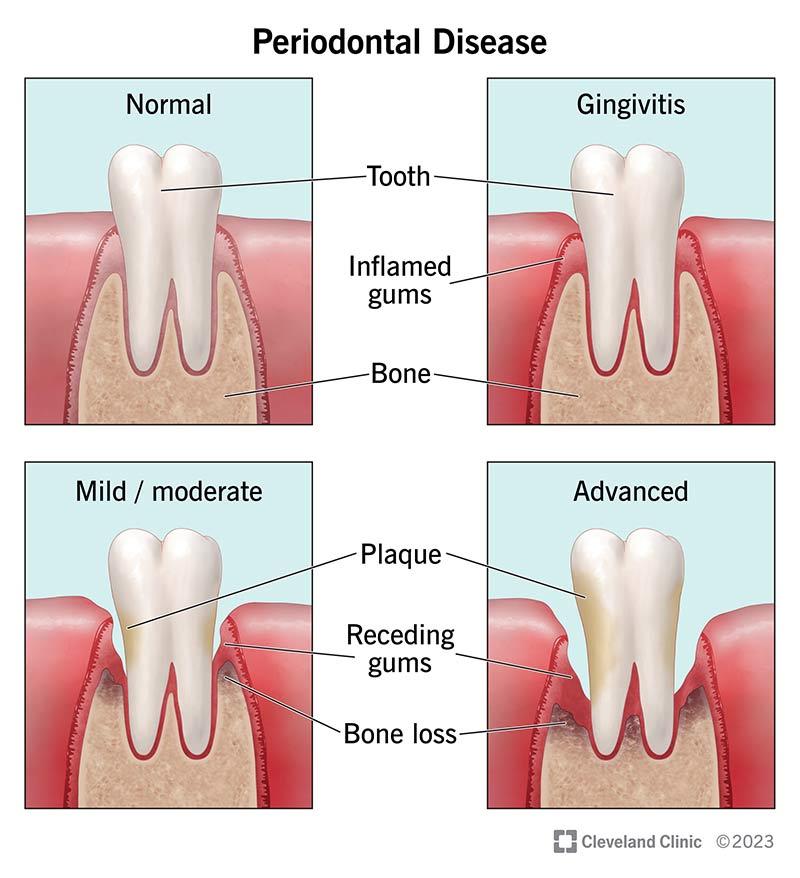
Periodontitis is a chronic inflammatory disease affecting the supporting structures of the teeth primarily the gums, periodontal ligaments, and alveolar bone. It is one of the most common oral health conditions worldwide and remains a leading cause of tooth loss in adults. While periodontitis often begins as gingivitis, or mild gum inflammation, it can progress into a far more destructive disease if left untreated. Beyond oral health, periodontitis has profound implications for systemic wellbeing, making its prevention and management vital for long-term health.
Understanding Periodontitis: Causes and Development
Periodontitis typically develops due to the accumulation of dental plaque, a sticky biofilm composed of bacteria, food debris, and saliva. When plaque is not removed through regular brushing and flossing, it hardens into tartar, which adheres strongly to teeth and irritates the surrounding gum tissue. The body’s immune response to the bacterial invasion leads to inflammation, and over time this inflammatory process destroys the connective tissue and bone that support the teeth.
Several risk factors increase the likelihood of developing periodontitis
-
Poor oral hygiene
-
Smoking or tobacco use
-
Diabetes
-
Genetic predisposition
-
Hormonal fluctuations, such as pregnancy or menopause
-
Stress
-
Medications that reduce saliva production
Although bacterial infection initiates the disease, the severity of periodontitis often reflects the individual’s immune response. In some people, even small amounts of plaque can trigger significant inflammation and damage.
Signs and Symptoms
Early detection is essential, but periodontitis often progresses silently. Common symptoms include:
-
Persistent bad breath
-
Red, swollen, or tender gums
-
Gum recession or the appearance of longer teeth
-
Bleeding during brushing or flossing
-
Loose or shifting teeth
-
Formation of deep periodontal pockets between teeth and gums
Because pain is not always present until the disease reaches an advanced stage, regular dental visits play a crucial role in early diagnosis.
Impact on Oral Health
Periodontitis can significantly compromise oral health in multiple ways
1. Tooth Loss
As the supporting bone deteriorates, teeth lose stability and may eventually fall out or require extraction. This not only affects appearance but also impairs chewing efficiency and speech.
2. Functional Decline
Without adequate support, chewing becomes painful or difficult. Individuals may avoid certain foods, leading to nutritional deficiencies.
3. Aesthetic Changes
Gum recession, tooth migration, and tooth loss can alter facial structure. Over time, the lower third of the face may appear sunken due to bone loss.
4. Increased Risk of Other Oral Conditions
Periodontitis can make individuals more susceptible to
-
Dental abscesses
-
Root sensitivity
-
Secondary infections
5. Complications for Dental Prosthetics
Removable dentures and other prosthetics rely on healthy gums and bone. Periodontitis reduces the stability of these devices, complicating dental rehabilitation.
Links Between Periodontitis and Systemic Health
Research continues to reveal strong associations between periodontal disease and numerous systemic conditions. Although causation is still under investigation, inflammation serves as a common thread.
Cardiovascular Disease
People with periodontitis have a higher risk of heart disease and stroke. Oral bacteria may enter the bloodstream and contribute to inflammation in blood vessels.
Diabetes
The relationship between diabetes and periodontitis is bidirectional. Poorly controlled diabetes increases the risk of gum disease, while periodontitis can make blood sugar levels harder to regulate.
Respiratory Illnesses
Bacteria from the mouth can be aspirated into the lungs, increasing the likelihood of pneumonia or worsening chronic respiratory disorders.
Pregnancy Complications
Severe periodontitis has been linked to preterm birth and low birth weight, likely due to systemic inflammatory responses.
Diagnosis and Treatment
Periodontitis is diagnosed through clinical examination, periodontal probing, and dental X-rays to assess bone loss. Treatment varies by severity and may include
1. Scaling and Root Planing
This deep-cleaning procedure removes plaque and tartar from below the gumline and smooths the root surfaces to discourage bacterial growth.
2. Antimicrobial Therapies
Dentists may prescribe topical or systemic antibiotics to reduce bacterial load. While medications serve specific roles, they are not a substitute for mechanical cleaning.
3. Surgical Interventions
For advanced cases, surgical procedures such as flap surgery, bone grafting, and tissue regeneration may be necessary to restore periodontal health.
4. Maintenance Therapy
Patients with a history of periodontitis require more frequent dental visits typically every three to four months to prevent recurrence.
Prevention: The Key to Long-Term Oral Health
Preventing periodontitis is far easier than treating its consequences. The following practices significantly reduce risk
-
Brush at least twice daily with fluoride toothpaste
-
Floss or use interdental cleaners daily
-
Limit sugary foods and drinks
-
Avoid tobacco products
-
Schedule regular dental checkups and cleanings
-
Manage underlying medical conditions, especially diabetes
Good oral hygiene and routine professional care remain the foundation of prevention.
The Role of Dental and Medical Supply Chains
Interestingly, the broader ecosystem supporting oral health includes not only dental professionals but also pharmaceutical suppliers, distributors, and wholesalers. In discussions of healthcare logistics, one might encounter diverse products from antiseptics to antibiotics distributed through channels that also handle unrelated medications. For example, a mebendazole wholesaler specializes in distributing antiparasitic medications, but such supply chains sometimes overlap with distribution networks for dental therapeutics, particularly in large-scale medical supply operations. While mebendazole itself is not used for periodontal treatment, its supply chain illustrates the complex network that ensures essential health products reach clinics and pharmacies efficiently.
Conclusion
Periodontitis is a serious and widespread condition with lasting implications for oral and overall health. Its progression from a mild gum infection to a destructive inflammatory disease can lead to tooth loss, aesthetic concerns, functional decline, and systemic complications. Fortunately, with early detection, proper treatment, and consistent preventive care, periodontitis can be managed effectively.
Understanding the importance of oral hygiene, maintaining routine dental visits, and addressing risk factors can dramatically reduce vulnerability to this disease. As awareness grows about the connections between periodontal health and broader wellness, the importance of oral care in everyday life becomes clearer than ever.